
Quick Links
Resources
About MyPsoriasisTeam
Powered By








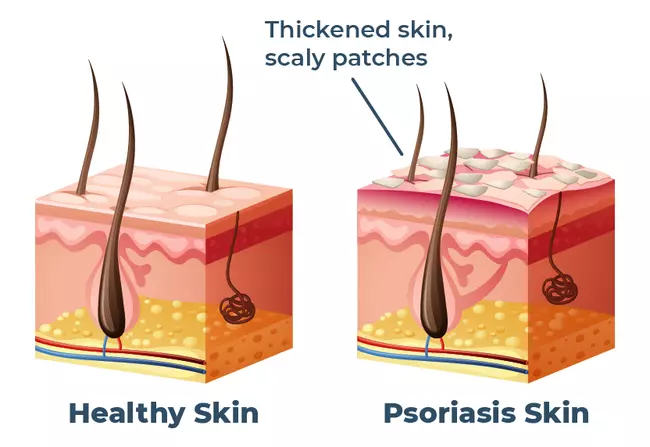 Psoriasis is a chronic autoimmune disease, which can be managed to reduce or prevent flare-ups. Psoriasis is caused by abnormal immune system reactions that result in inflammation of the skin. The most common form of the condition, plaque psoriasis, causes skin cells to rapidly overproduce and build up in thick, scaly patches or lesions that can become itchy and sore.
Psoriasis is a chronic autoimmune disease, which can be managed to reduce or prevent flare-ups. Psoriasis is caused by abnormal immune system reactions that result in inflammation of the skin. The most common form of the condition, plaque psoriasis, causes skin cells to rapidly overproduce and build up in thick, scaly patches or lesions that can become itchy and sore.
Psoriasis tends to flare in cycles. Flare-ups may last for weeks or months, and then the condition often calms down or goes into remission. During flares, symptoms worsen and quality of life can be severely impacted, affecting both physical and emotional well-being. Taking measures to prevent flares can help keep the condition from becoming debilitating and impeding daily activities.
Psoriasis affects everyone differently, and what works for one person may not work for everyone, but there are effective ways to help prevent flare-ups.
Stick To Your Treatment Plan |
Treatment for psoriasis can include topical steroids and moisturizing ointments, gels, lotions, or shampoos. It may also incorporate light therapy (phototherapy), oral medications, and injections or infusions. Your doctor may prescribe treatment regimens with the goal of managing psoriasis flare-ups or maintaining remission. Treatment may involve prescription medication or over-the-counter moisturizers.
First and foremost, it’s essential that you adhere to your psoriasis treatment plan as a first line of defense against flare-ups. Avoid making adjustments to your treatments without consulting your doctors first. Studies have shown that people with psoriasis have a low rate of adherence to treatment plans, due to factors such as dissatisfaction with treatment effectiveness, problematic relationships with doctors, and personal motivation.
 Your risk for flare-ups may increase if you do not stick with your treatment plan. If you are unhappy with your treatments, it’s important to talk to your doctor to determine what your options are, rather than stopping treatment on your own.
Your risk for flare-ups may increase if you do not stick with your treatment plan. If you are unhappy with your treatments, it’s important to talk to your doctor to determine what your options are, rather than stopping treatment on your own.
Symptom Diaries for Psoriasis |
A symptom diary may help you and your health care team monitor symptoms, identify triggers, and anticipate flares, based on day-to-day activity. Diaries can also be used to keep track of everything you eat and drink to determine if any foods are triggering flares.
Clinical tools have been developed to help people with psoriasis monitor and report symptoms over time. The Psoriasis Symptom Diary was created to track the daily experiences of people with psoriasis to determine the severity of symptoms, such as itching, stinging, bleeding, and joint pain. The Psoriasis Symptom Inventory is a questionnaire that can be used to monitor experiences with psoriasis and changes in skin condition. You may want to talk to your doctor about the benefits of keeping a daily diary of your symptoms, as a tool to potentially prevent flare-ups.
A number of mobile apps are also available to help people with psoriasis monitor disease activity, track their diets, or adhere to treatment. However, not all apps are based on clinically established measures. If you are interested in using an app to track your condition, talk to your health care team to determine which app might be best for you.
Understand Flare-Up Triggers |
MyPsoriasisTeam members often discuss flare triggers. “I have found that any virus triggers my psoriasis. If my body isn't happy, neither is my skin. Eating clean helps me, too,” said one MyPsoriasisTeam member. “I’m learning that stress seems to be the major trigger for my psoriasis,” wrote another.
 “I’m testing out my triggers,” a member said. “I think red wine and I don't mix.”
“I’m testing out my triggers,” a member said. “I think red wine and I don't mix.”
A number of common triggers can cause flares in some people with psoriasis. By increasing your awareness of triggers, you can help avoid some of the factors that may worsen psoriasis symptoms.
Psoriasis is associated with an increased risk for depression and stress, which can trigger flares or worsen symptoms. Managing stress can help prevent flares. Some techniques you can use to decrease stress, include:
Talk to your doctor if stress is negatively impacting your life. They can recommend the safest exercise plan for you, or make a referral to a mental health provider, if necessary.
Cuts, scrapes, scratches, sunburns, and bug bites are all common causes of psoriasis flares. As much as possible, try to avoid situations that can injure your skin. Avoid scratching your skin, which can cause injury and increase the chance of infection.
Some medications are associated with an increased risk of flares. High blood pressure medications, such as beta-blockers; antimalarial medications; and lithium, which is sometimes used to treat bipolar disorder, are some of the drugs associated with flare-ups.
Talk to your dermatologist about all of the medications you are taking to determine if any of them might be associated with flares. Consult with all of your doctors, including your primary care physician, before changing any medications.
Tobacco smoking and exposure to tobacco smoke can trigger psoriasis flares. If you smoke, talk to your doctor about safely quitting. Nicotine patches have been associated with psoriasis flares and should be avoided. If you live with someone who smokes, let them know that smoke is problematic for people with psoriasis and identify ways to minimize your exposure.
Excessive alcohol use is also associated with flare-ups and may be a factor in setting off inflammation and making it worse. Alcohol can interact adversely with medication and is associated with increasing susceptibility to infection. If you consume alcohol, moderate your drinking and take note if it aggravates your psoriasis. Talk to your doctor if you have concerns about your alcohol consumption.
Some people with psoriasis find that dry, cold weather triggers psoriasis flares. Both indoor heat and air conditioning can also cause dry skin that may put you at risk for a flare-up. A humidifier can help with dry air indoors.
While sunlight and humidity are associated with benefits for psoriasis, sunburn can injure your skin and should be avoided. Use sunscreen when spending prolonged time in sunlight.
Learn more about weather and psoriasis flares.
A healthy diet — such as the Mediterranean diet — rich in vegetables and fruits, fish, whole grains, and extra-virgin olive oil has been found to have anti-inflammatory effects and may reduce severe flares. Read more about anti-inflammatory diets for psoriasis.
Some people with psoriasis are sensitive to gluten, a protein found in wheat, rye, barley, triticale, and brewer’s yeast. One study found people with psoriasis were three times more likely to have celiac disease — a condition caused by gluten intolerance — than the general population. If you suspect you may be sensitive to gluten, avoid products with gluten. You can also ask your doctor to consider testing you for celiac disease.
Strep throat and viral infections, such as flu or cold, may also trigger flare-ups in people with psoriasis. While infections cannot always be prevented, if you feel you are getting sick, you may want to take extra precautions to avoid worsening the infection.
Join a Supportive Community |
By joining MyPsoriasisTeam, you become part of a supportive community of more than 86,000 people who are managing psoriasis. Share experiences and tips on how to prevent flares. Ask questions about triggers and what people do to avoid them.
What triggers psoriasis flare-ups for you? Do you keep a symptom diary to help avoid flares? Share in the comments below or join MyPsoriasisTeam and start a new conversation today.
Get updates directly to your inbox.



Sign up for free!
Become a member to get even more




A MyPsoriasisTeam Member
I've had a really massive flare up after having a, shingles vaccination.
We'd love to hear from you! Please share your name and email to post and read comments.
You'll also get the latest articles directly to your inbox.